from the archives
Well that sounds familiar
U.S. News & World Report
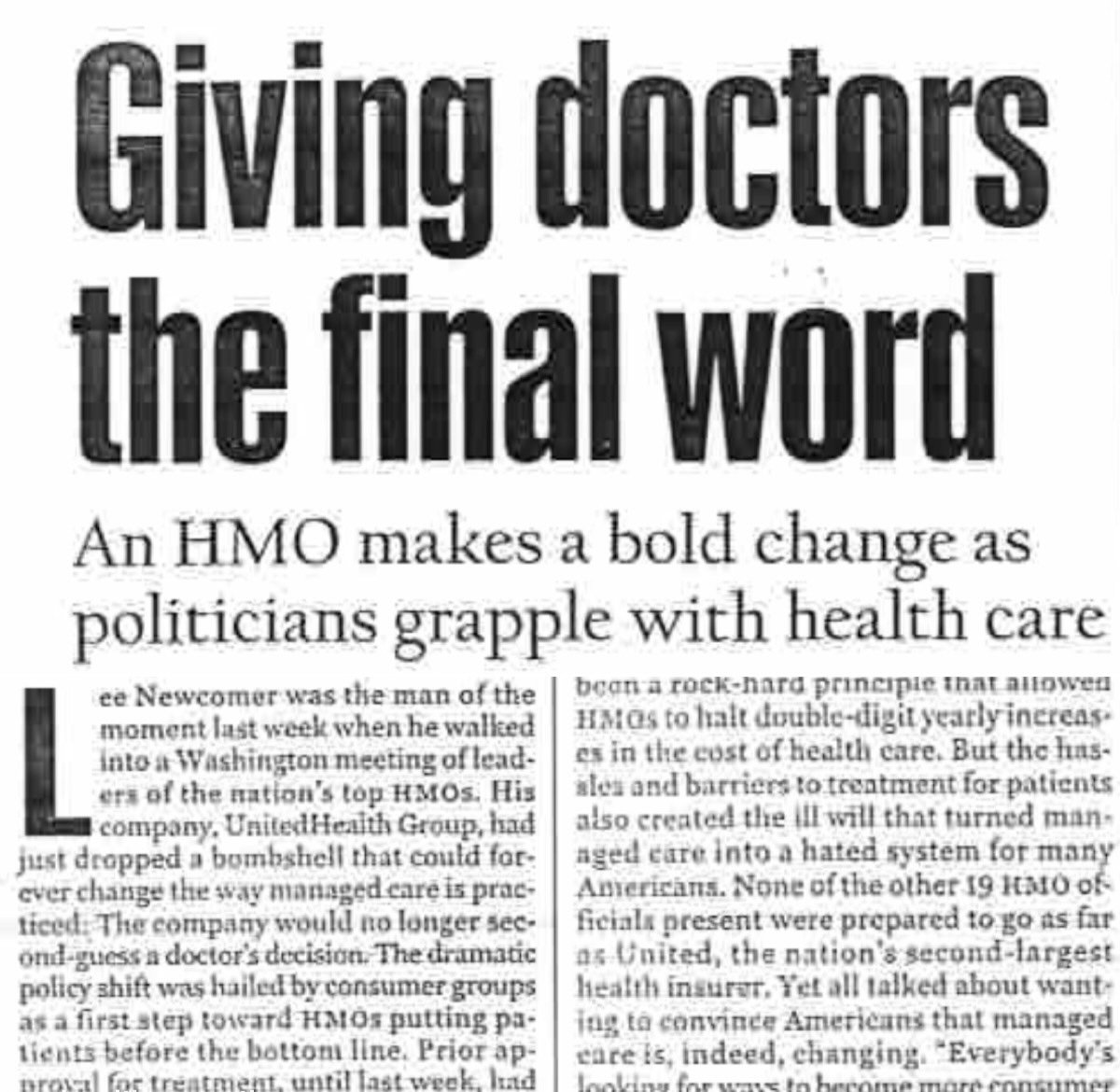
The Trump administration made a big show of last week’s announcement that health insurers were making a voluntary pledge to scale back their use of prior authorizations. We’ve heard these pledges before.
Yes, these same groups made almost identical promises back in 2018. A friendly Health Care Inc. reader also passed along the above article from U.S. News & World Report, published in November 1999. The Wall Street Journal had a write-up, too. Same exact stuff, 26 years apart.
spending
$5.3 trillion
That’s how much America spent on health care in 2024, according to the newest estimates from federal actuaries. That spending total was 8% higher than in 2023. The $5.3 trillion health care tab now represents 18% of the entire economy, up from 17.6% in 2023.
These government reports are vital. They give a snapshot of what the health care economy looks like and why certain parts are getting more expensive than others. Although the long-term predictions are, understandably, wrong all the time, it’s most useful to understand what happened most recently. And it’s clear that spending on hospitals (9.2%), medical groups (8.1%), and pharmaceutical manufacturers (10.1%) increased at rates well above inflation.



