consolidation
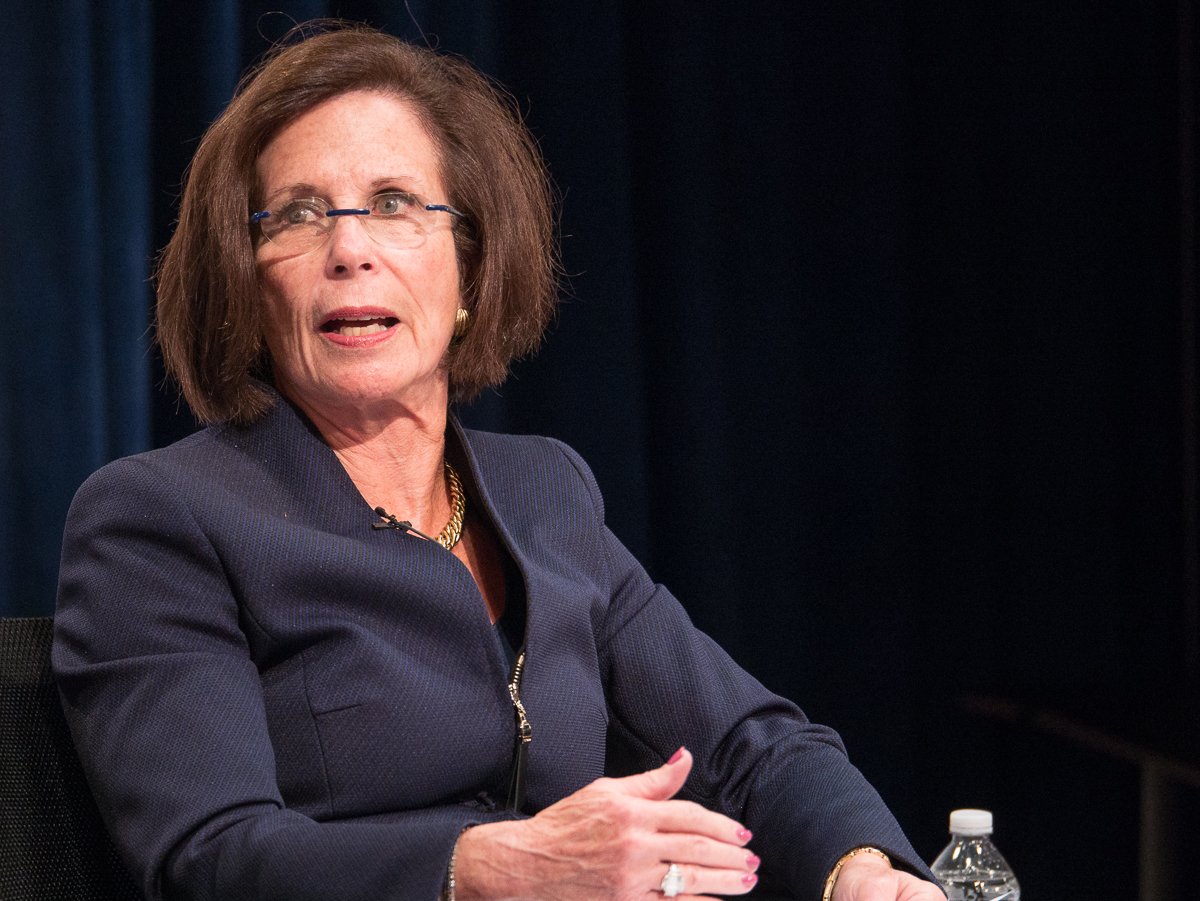
Gail Wilensky on Geisinger’s sale to Kaiser
Karl Eisenhower/Alliance for Health Reform
No deal is bigger in health care right now than Kaiser Permanente’s takeover of Geisinger. It came out of nowhere and will lead to the formation of a new national mega-system of integrated health systems. Naturally, people want to know which dominoes are next to fall into this organization, called Risant Health. But an even more basic question keeps coming to the fore: Why?
Well, a major impetus that pushed Geisinger was the relentless consolidation of its competitors, particularly UPMC and Highmark, Geisinger board member Gail Wilensky said in an interview. It’s an answer that could foreshadow which systems are eager to join.
“There have definitely been a lot of acquisitions and mergers. UPMC has been quite aggressive,” said Wilensky, who also was the former CMS administrator under President George H.W. Bush. “For Geisinger, it was really a cultural issue of what’s important to the organization. How do we find like-minded groups that we might consider to partner with?”
Read our entire conversation where Wilensky answers a slew of questions about what brought this deal about, the concerns around consolidation, and whether “value-based care” is baloney.
earnings
Potent quotables
Last week was chock full of health care earnings calls. It also included a big home care merger between Option Care Health and Amedisys. But I wanted to highlight two quotes from health care executives that sum up some big themes in the air.
Cigna: The company is immensely profitable, thanks in large part to the pharmacy benefit manager it acquired a few years ago, Express Scripts. CEO David Cordani, the king of corporate jargon (he uttered the word “value” 25 times throughout the earnings call), said 20% of Express Scripts’ pre-tax profits come from rebates and spread pricing. That percentage has been declining over time, and Cordani believes Cigna is ready if Congress passes PBM reforms:
“We are confident that we will be able to flex rapidly, if necessary. But we want to also ensure that we are a voice for employers to still work to preserve choices for them, as how they want to finance their programs, how they want to manage their overall cost and predictability from that standpoint. But to reassure you, we have ample flexibility to flex rapidly.”
Community Health Systems: The hospital chain lost more money in the first quarter, and executives made sure to note that Medicare Advantage plans are a thorn in their side. Patient volumes increased, and most of the increase came from MA patients. Some research has suggested MA plans pay providers “nearly identical” rates as traditional Medicare, while other studies suggest MA plans pay providers up to 8% less than traditional Medicare. Comments from CFO Kevin Hammons fall on the latter view, and indicate MA plans may be paying even less now:
“We’re seeing … between 85% and 90% payment for MA patients compared to Medicare fee-for-service.”
hospitals
The hospital lightning round
Several not-for-profit hospital systems posted first-quarter financials in the past week as well. A few trends are coming through: Revenues are higher because patient volumes are back; expenses are higher because hospitals raised employees’ wages and needed more supplies to account for the increased volumes; contract labor is definitely less of a thing; and Wall Street investments are doing very well again.
- BayCare Health System: Patients flocked back to the Florida-based system, which operates 16 hospitals. The operating margin (4.6%) was actually down a little year over year because BayCare recorded higher employee costs.
- Indiana University Health: The academic system is back in the black and recorded much higher gains from Wall Street investments, and it also disclosed it will issue more than $750 million of new debt this year. Surgeries increased more than 16% year over year across IU Health in the quarter.
- Sanford Health: Admissions and outpatient visits bucked the trend and fell in Sanford’s first quarter this year, while ER visits and surgeries increased modestly. Sanford is still in the process of trying to merge with Fairview Health Services
- Sutter Health: The California-based giant registered a 5.1% net margin, making it less profitable than other similarly sized hospital systems.
- University of Louisville Health: Elevance/Anthem is a major source of revenue for this profitable academic system. A routine footnote in the financial document reiterates how U of L Health’s contracts with Anthem include “automatic renewals with annual negotiated payment updates.”



