first opinion
A rehabilitation researcher transformed by his daughter's traumatic brain injury

Lindsay Sulzer
James Sulzer hopes no one else comes to know the drastic consequences of a neurological injury the way his family has. In 2020, his almost 4-year-old daughter Livie sustained a severe traumatic brain injury when a tree branch fell on her head in their backyard, devastating the whole family. After five months in the hospital, she had become cognitively impaired and couldn't walk, talk, or do any activities on her own. As a rehabilitation researcher for two decades, Sulzer found his professional background helped far less than he had expected.
“The emotional, logistical, and physical toll of Livie’s care, coupled with the realization of just how limited my research expertise is to help her, has been soul-sapping,” he writes in a STAT First Opinion. “We need to include input, experiences, and insights from people affected by conditions like brain injury in the entire research process.” Read more.
health
Older patients spend three weeks a year getting health care away from home
Back in June 2020, I visited a cancer center with a patient participating in a clinical trial to treat her ovarian cancer. Because Covid-19 was fairly new and vaccines were still far away, great efforts were made to streamline visits so no patient was exposed longer than necessary to other people. That came to mind as I read a study in this week's Annals of Internal Medicine tracking just how much time older patients who still live independently spend getting health care outside their homes.
The average was three weeks a year in the cross-sectional study of more than 6,500 adults 65 and older (and 50 days for 11% of them). Here’s what made me recall the cancer story: About half of the older patients’ test days and imaging days were not on the same days as office visits, which doesn’t sound like streamlined care. But an editorial hints that could change: “Policymakers and health care systems are increasingly using measures that more fully capture what matters most to many older adults — the amount of time they spend outside of the health care system.”
health equity
Black people enrolled in Medicaid have more preventable hospitalizations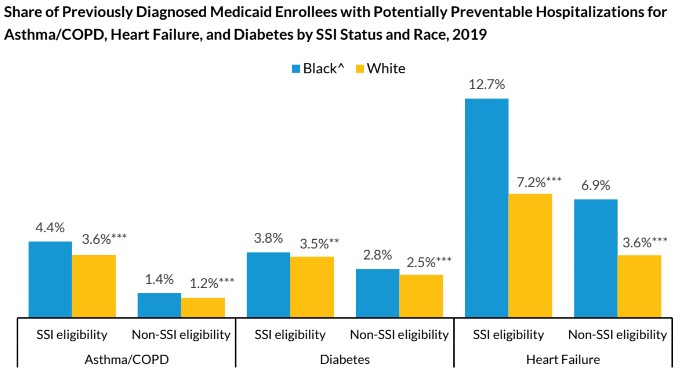
Urban Institute
Not every hospital admission has to happen. They can often be prevented — in up to 3.5 million cases, one annual estimate says — if patients can find timely, high-quality outpatient care. A new analysis from the Urban Institute has found that Black people enrolled in Medicaid have higher rates of preventable hospitalizations than white people covered by Medicaid. Looking at 21 U.S. states, three previously diagnosed conditions were most likely to result in a hospital stay: asthma or chronic obstructive pulmonary disease, diabetes, and heart failure.
Hospitalization rates were higher for people insured by Medicaid through the Supplemental Security Income program, which is based on a qualifying disability, but for heart disease in particular, Black Medicaid enrollees were more likely to have a preventable hospitalization than white enrollees, with or without SSI, the report found. “These findings suggest a need to improve access to outpatient care to effectively manage chronic conditions,” the report concludes.